This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
41 year old male, petrol pump operator by profession resident of narketpally.
Chief complaint:
Shortness of breath since 15 days
Abdominal distention since 15 days
5-6 episodes of vomiting 6 days ago.
HOPI :
patient was apparently asymptomatic 15 days back when he developed shortness of breath which was sudden in onset and increased on activity. (Grade 3)
He also developed abdominal distention 15 days ago.
He developed nausea and had 5-6 episodes of vomiting which was sudden in onset.
Patient came to the hospital where he was admitted.
There were 5-6 episodes after consumption of water. Last meal was taken at lunch in the previous day.
Episodes were non projectile, non bile stained or blood stained.
There was no fecal smell associated with the vomitus. There is history of apparent weight loss of around 4-5 kgs in the past 6 months reported by the attender.
There is history of alcohol consumption prior to the vomitings.
Patient reported similar cases of vomiting 2-3 months back, when alcohol was consumed.
No history of fever, stomach pain, loose stools.
No symptoms indicative of raised ICP.
PAST HISTORY
Patient is a k/c/o DM, HTM
DM : since 3 years
HTN : since 3 years
Which were both discovered when pt suffered a leg injury which led to hospitalization.
He has been on medication for the same since then.
Not a k/c/o of asthma, TB, Epilepsy.
PERSONAL HISTORY
Diet : Mixed
Appetite: Normal
Bowel & Bladder: regular
Sleep : Adequate
Addictions :
• Alcohol consumption since 8-9 years, on a regular basis (daily)
He had stopped consumption for a month after the previous episode 2-3 months ago, and consumed it again 7 days back.
GENERAL EXAMINATION
Patient is c/c/c well oriented to time, place and person.
Moderately built and nourished.
Pallor & Icterus were seen
No Cyanosis, Clubbing, Lymphadenopathy.
vitals :
BP: 120 / 70 mmHg
Pulse : 72 BPM
Respiratory rate : 20cpm
Temp: 98.5° F
GRBS: 161 mg/dl
CVS : S1S2 heard
Respiratory: BAE + NVBS heard
CNS : No focal neurological deficit.
Abdomen : Soft, Non tender
Shape : DISTENDED.
Umbilicus:inverted
Skin over the abdomen is shiny
All quadrants are moving equally with respiration
No visible peristalsis, Hernial orifices are intact
Visible superficial abdominal vein running vertically down is seen
External genitalia normal
Fluid thrill present.
On percussion Shifting fluid sign present.
INVESTIGATIONS:
1. USG LIVER
2. ECG
3. 2D ECHO
PROVISIONAL DIAGNOSIS :
ALCOHOLIC LIVER DISEASE
TREATMENT:
DAY1
1) Tab PAN 40 mg | PO/OD 7AM
2) Tab. ODILIV 300mg PO/BID
3) SYP. HEPAMER 15 mL | PO/TID
4) Syp. LACTULOSE PO/OD 15ml in glass of water
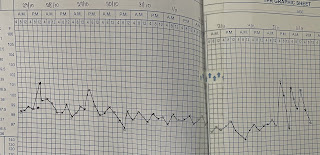
5) GRBS PROFILE MONITORING.
6) BP, PR, RR MONITORING 4th hourly
7) tab- glimiperide PO / OD /8AM
8) Tab AMLODIPINE [PO/ OD 8 AM]
DAY 2
1) Tab PAN 40 mg | PO/OD 7AM
2) Tab. ODILIV 300mg PO/BID
3) SYP. HEPAMER 15 mL | PO/TID
4) Syp. LACTULOSE PO/OD 15ml in glass of water
5) GRBS PROFILE MONITORING.
6) BP, PR, RR MONITORING 4th hourly
7) tab- glimiperide PO / OD /8AM
8) Tab AMLODIPINE [PO/ OD 8 AM]
DAY 3
1) Tab PAN 40 mg | PO/OD 7AM
2) Tab. ODILIV 300mg PO/BID
3) SYP. HEPAMER 15 mL | PO/TID
4) Syp. LACTULOSE PO/OD 15ml in glass of water
5) GRBS PROFILE MONITORING.
6) BP, PR, RR MONITORING 4th hourly
7) tab- glimiperide PO / OD /8AM
8) Tab AMLODIPINE [PO/ OD 8 AM]













Comments
Post a Comment